
Transcription
Comment Response
Dear Susan,
Greetings. I am grateful that there is someone deeply interested in the connection between criminal behavior and mental illness. This is a subject that hits home with me. I was diagnosed with bipolar disorder at age 15 and made my rounds in the psych units both before and during my prison sentence (see my recent post on this subject).
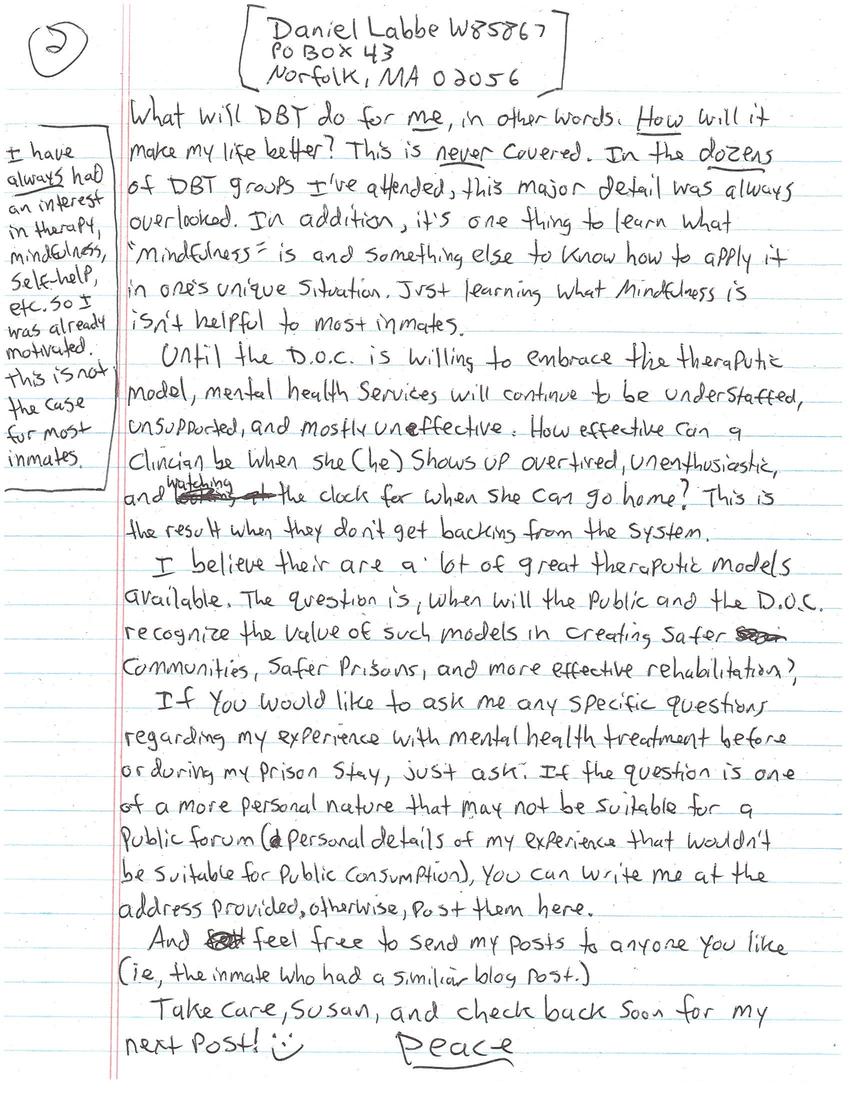
The amount of people on psychotropic drugs in prison is huge. Sadly, the drugs are used as a management tool rather than as therapeutic treatment for the inmate. [I WAS fortunate enough to have a clinician for two years who was deeply dedicated and helpful. Sadly, she found work elsewhere. This is the rare exception, NOT the norm.] There is mental health access in prisons, but they are so understaffed and unsupported by the administration that all they are able to do is manage crisis situations. "Therapy" is NOT available, unless you count seeing a clinician once every 4-6 weeks for 20-30 minutes therapy. Some prisons, like Old Colony in Bridgewater, MA, offer group therapy. What they teach is good, up to date material, but due to being understaffed and unsupported, groups are OFTEN cancelled, rushed through, or dropped altogether. In addition, the material is merely presented rather than taught. Take DBT (dialectical behavior therapy) for example. The material is GREAT. If learned and applied inmates could benefit tremendously (as I did). The problem is, most inmates don't have the skills to learn new information then apply it to their own unique situation. They need to first know WHY they should even care. What will DBT do for ME, in other words. HOW will it make my life better? This is NEVER covered. In the DOZENS of DBT groups I've attended, this major detail was always overlooked. In addition, it's one thing to learn what "mindfulness" is and something else to know how to apply it in one's unique situation. Just learning what mindfulness is isn't helpful to most inmates.
[I have ALWAYS had an interest in therapy, mindfulness, self-help, etc. So I was already motivated. This is not the case for most inmates.]
Until the D.O.C. is willing to embrace the therapeutic model, mental health services will continue to be understaffed, unsupported, and mostly ineffective. How effective can a clinician be when she (he) shows up overtired, unenthusiastic, and watching the clock for when she can go home? This is the result when they don't get backing from the system.
I believe there are a lot of great therapeutic models available. The question is, when will the public and the D.O.C. recognize the value of such models in creating safer communities, safer prisons, and more effective rehabilitation?
If you would like to ask me any specific questions regarding my experience with mental health treatment before or during my prison stay, just ask. If the question is one of a more personal nature that may not be suitable for a public forum (personal details of my experience that wouldn't be suitable for public consumption), you can write me at the address provided, otherwise, post them here.
And feel free to send my posts to anyone you like (i.e., the inmate who had a similar blog post.)
Take care, Susan, and check back soon for my next post! :) Peace.
Other posts by this author
|
2016 aug 4

|
2016 jun 25

|
2016 jun 9

|
2016 may 5

|
2016 mar 11

|
2016 feb 7

|
More... |



Replies